
Soon after the World Health Organization declared COVID-19 a global pandemic, Americans became aware that a “new normal” was about to supplant their daily lives.
This was a particularly grim reality for those considered most vulnerable if infected by the coronavirus: people age 65 and older, and those with pre-existing medical conditions. Securing health, wellness, and everyday household items gained widespread attention as citizens were informed to take preventative actions and prepare for possible illness. The apprehension in the ability to secure healthcare items had many Americans reviewing their options for alternative ways to prepare themselves, and proactively protect against the coronavirus and/or prevent transmission.
For 80 percent of the 22 million Medicare Advantage (MA) enrollees, a selection of health and wellness products are available as an over-the-counter benefit (OTC). Convey Health Solutions, Inc. (Convey) is a leading provider of supplemental over-the-counter benefit administration services, and core to those services is the company’s member advocates whom provide support and outreach to Medicare beneficiaries with access to these allowances. Among the 400+ benefit configurations managed by Convey for their MA plan clients, benefits amounts can range from $10 - $75 per month and $10 - $350 per quarter.
Heightened concern about obtaining important health, wellness, and everyday household products led to a considerable surge in overall benefit utilization, and in turn, call and shipping center volume at Convey’s contact and distribution centers. In just the first three days of April, Convey received approximately 30 percent of the entire month’s call volume. “We had to take immediate steps to address the call volume and be able to support our beneficiaries so they could obtain necessary products from the safety of their homes,” said Melissa Murray, Convey’s Vice President of Operations.

Many of Convey’s customers shifted quickly to online and mobile purchasing for a more convenient experience. The shift to digital tools by members was more rapid than what was experienced in years past, and this was clear in reviewing the data. The response was significant. Web utilization nearly doubled from an average of 27 percent to 52 percent. Use of the company’s new mobile application, OTC-Anywhere, also showed a considerable uptick. Once customers, who had grown very accustomed and comfortable placing their order on the phone or using a mail order form, became familiar with the online process they adopted and remained active with the digital tools.
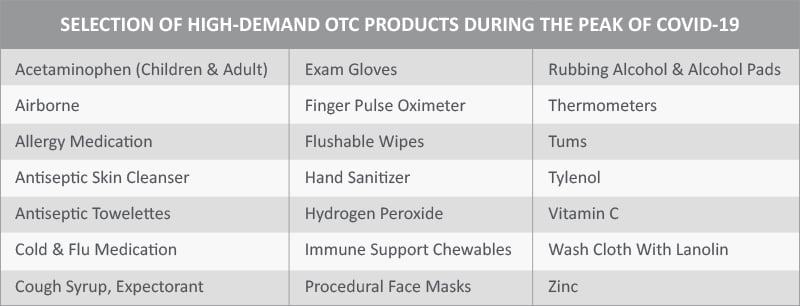
As orders continued to rise, Convey monitored trends related to the pandemic. One trend that presented because of limited supplies, nation-wide, of high-demand products, was creative ways of making hand sanitizer at home through combining rubbing alcohol and aloe vera. It was also clear that members were nervous entering retail stores for fear of potential exposure to infected individuals. Throughout the pandemic, members considered visiting retail stores to be a high-risk activity.
“Shopping in retail stores was especially risky for the vulnerable population we serve,” Murray said, “so we provided options to reduce the need for members to leave their homes. Our focus is to keep them safe while obtaining the items they need.”
Other digital tools provided by Convey included an online “click-to-chat” feature for customers who had a question while accessing the online environments and improved interactive voice response (IVR) for intelligently routing customers to more productive agents and to educate or remind members of the online and mobile ordering options.
Through these digital solutions as well as rapid response to the pandemic, Convey returned to meeting daily customer service targets and maintained service levels for health plan clients.
In anticipation of another rise in call volume at the start of the new quarter in July, and with COVID-19 still a global and national disruptor, Convey is supporting proactive outbound campaigns to contact beneficiaries and encourage them to “beat the rush” and order necessary supplies in advance. These efforts, and the overall benefit utilization increase across all of the Convey-administered health plan beneficiaries, necessitated the hiring of additional team members and revised training curricula for OTC advocates. To mitigate health risks posed by COVID-19 and maintain social distancing, Convey employed the use of several virtual recruitment tools to supplement their in-person recruitment and hiring efforts: interviewing through online meeting platforms and setting up online training sessions.
COVID-19 has triggered the need for innovative solutions throughout many industries and businesses. For Convey, innovation and agility have been the key elements to its very successful operational enhancements during the pandemic.
In relation to COVID-19, 60 percent of privately insured U.S. health plan members said they were not contacted by their health plan with guidance or information, and 48 percent said their health plan had not shown concern for their health since the pandemic began. Understanding also that effective communication geared towards overall customer satisfaction is a weak point for many Medicare Advantage plans, further amplified by the pandemic, Convey chose a pre-emptive path and chose to focus on member satisfaction through this crisis.
“We know that higher utilization of a plan’s OTC benefit program contributes to improved member health, satisfaction, and reductions in costs of care,” Murray said. “At Convey, we have always put the best interests of our members first and strive to be a dedicated resource for them,” Murray said. “Customer support and engagement is at the heart of our services.”
Learn more about Convey's OTC home delivery services that have supported members for 10+ years.
To learn about the other Medicare supplemental benefit programs offered by Convey, visit conveyhealthsolutions.com/medicare-supplemental-benefits/
Read about how our IT team navigated the complexities of COVID-19 by transitioning 1,000+ of our team members from our physical locations, to their homes.
- https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/checklist-household-ready.html
- https://www.palmbeachpost.com/news/20200501/coronavirus-florida-some-medicare-advantage-plans-allow-for-mask-purchases
- https://www.jdpower.com/business/press-releases/2020-us-commercial-member-health-plan-study
- https://www.jdpower.com/business/press-releases/2020-us-medicare-advantage-study





